
* Declaration; I have published articles with two of the authors of this article, including on this topic, and know most of them professionally
One influential model of the onset of psychotic disorders such as schizophrenia is the stress-vulnerability model, first put forward by Zubin and Spring in 1977. This model proposes that people at risk for psychosis have various vulnerability factors, which could include a family history of schizophrenia, early childhood trauma, or high levels of cannabis use. However, this combined vulnerability is not revealed unless there is a significant stress event in later life.
Although stress can be either physical or psychological, the biological response is the same and is mediated through the hypothalamus-pituitary-adrenal (HPA) axis. The hypothalamus stimulates the pituitary, which produces a hormone that results in cortisol being released from the adrenal glands. High levels of cortisol are known to cause structural brain changes and may also be associated with poor physical health and increased risk for suicide.
While it is possible to measure cortisol in blood or saliva samples, these can sometimes be difficult to obtain, and because cortisol levels fluctuate over the day (being highest soon after waking) differences between populations can be related to altered sleep patterns or poor compliance with the specific timing of collection. An alternative approach is to measure the size of the pituitary directly, because there is evidence that increased size is related to greater activation of the HPA axis. This can be done using standard brain imaging techniques, which has the added advantage of allowing investigation of stress in previously collected cohorts who lack blood or saliva samples.
Although there have now been several studies examining pituitary volume at various stages of psychotic illness, there has been no previous systematic review. This meta-analysis, by Nordholm and colleagues, is therefore a useful attempt to set out to the evidence for either increased or decreased pituitary volume in people with schizophrenia or at risk of developing a psychotic disorder.
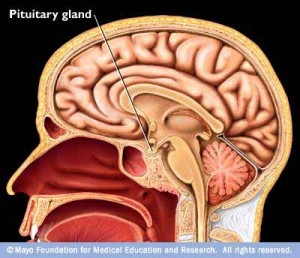
The pituitary gland produces a hormone that results in cortisol being released from the adrenal glands
Methods
The authors conducted a search of the PubMed, EMBASE, PsychInfo, Cinahl, and Science Citation Index Expanded (Web of Science) databases for publications that used one of the following terms; schizophrenia, ultra high risk, psychosis, schizotypal, at risk mental state, pituitary, HPA and hypophysis. They subsequently hand-searched reference lists and asked other experts about further studies, and also searched for unpublished trials on PROSPERO (a register of systematic reviews).
19 articles were identified that compared pituitary volumes between control participants and either individuals at clinical high-risk for psychosis, patients in their first episode of a psychotic illness, or patients with established schizophrenia. These articles reported findings from 13 studies, one of which was unpublished and could not be included, and two others which were follow-ups of subjects included in other papers.
Results
The meta-analysis assessed 10 studies that included 1,451 participants, made up of 177 at risk individuals, 617 first episode or established schizophrenia patients, and 657 controls.
- No significant difference in pituitary volume was found for either:
- the at risk group (standard difference in means (SDM) = 0.25, 95% CI -0.17 to 0.66, p=0.24)
- or the first episode/schizophrenia group (SDM = 0.10, 95% CI -0.20 to 0.40, p=0.52)
- However, when at risk subjects who later transitioned to psychosis were compared against controls (only two studies), there was weak evidence for pituitary enlargement in the at risk group (SDM = 0.37, 95% CI 0.0 to 0.75, p=0.05)
- There was significant evidence for an impact of antipsychotic medication on pituitary volume, with the inclusion of medicated patients being associated with increased volume
Overall, heterogeneity between studies was high, and there were important methodological differences. For example, different studies presented different information about how long patients had been unwell, and reliability of pituitary volume measurement varied widely.

No significant difference in pituitary volume was found for either the at risk group or the first episode/schizophrenia group
Strengths and limitations
- The authors have been thorough in searching for relevant published studies
- Good attempts have been made in analysis to investigate the confounding effects of gender and medication use
- Pituitary volume has not been validated as a measure of HPA activation with other measures (such as blood cortisol or perceived stress)
- The number of at-risk participants is small, and the number who have transitioned to psychosis even smaller, making the findings related to these groups unreliable
Conclusion
Pituitary volume does not seem to be affected in people with first episode psychosis or schizophrenia, and there is only very limited evidence that there is pituitary enlargement (and therefore increased biological stress) in individuals before the onset of disorder. Although pituitary volume remains a straightforward way to measure stress and HPA activation, its direct relationship with other stress measures in psychotic disorders (both psychological and biological) is not at all clear.
Links
Nordholm, D., et al., Pituitary gland volume in patients with schizophrenia, subjects at ultra high-risk of developing psychosis and healthy controls: A systematic review and meta-analysis. Psychoneuroendocrinology (2013), http://dx.doi.org/ 10.1016/j.psyneuen.2013.06.030 [PubMed abstract]
Further reading
Bradley AJ, Dinan TG. A systematic review of hypothalamic-pituitary-adrenal axis function in schizophrenia: implications for mortality. J Psychopharmacol. 2010 Nov;24(4 Suppl):91-118. doi: 10.1177/1359786810385491. [PubMed abstract]
Phillips LJ, McGorry PD, Garner B, Thompson KN, Pantelis C, Wood SJ, Berger G. Stress, the hippocampus and the hypothalamic-pituitary-adrenal axis: implications for the development of psychotic disorders (PDF). Aust N Z J Psychiatry. 2006 Sep;40(9):725-41.
Zubin, J., Spring, B., 1977. Vulnerability: a new view of schizophrenia (PDF). J. Abnorm. Psychol. 86, 103—126.


Meta-analysis finds that pituitary volume is not affected in people with first episode psychosis or schizophre… http://t.co/tY94vMSZTO
Reads like debunking of the 1977 hypothesis and ultimately they were more derogative about weed back then
@StephenWood8 highlights research showing that ppl with schizophrenia have no significant diff in pituitary volume http://t.co/eaz4DBH0Zg
Systematic review finds significant evidence for an impact of antipsychotic medication on pituitary volume http://t.co/eaz4DBH0Zg
Don’t miss: Review finds that pituitary volume is not affected in ppl w/ first episode psychosis or schizophrenia http://t.co/eaz4DBH0Zg
@Mental_Elf good to know, I work in an early intervention in psychosis team so will forward to colleagues
Mental Elf: Meta-analysis finds that pituitary volume is not affected in people with first episode psychosis or… http://t.co/M957HvVfsA
Meta-analysis finds that pituitary volume is not affected in people with first episode psycho… http://t.co/qs3rnHwcyO